Lily’s nursing journey at Pilgrims Hospices: “I’m lucky and honoured to be part of such an incredible team”

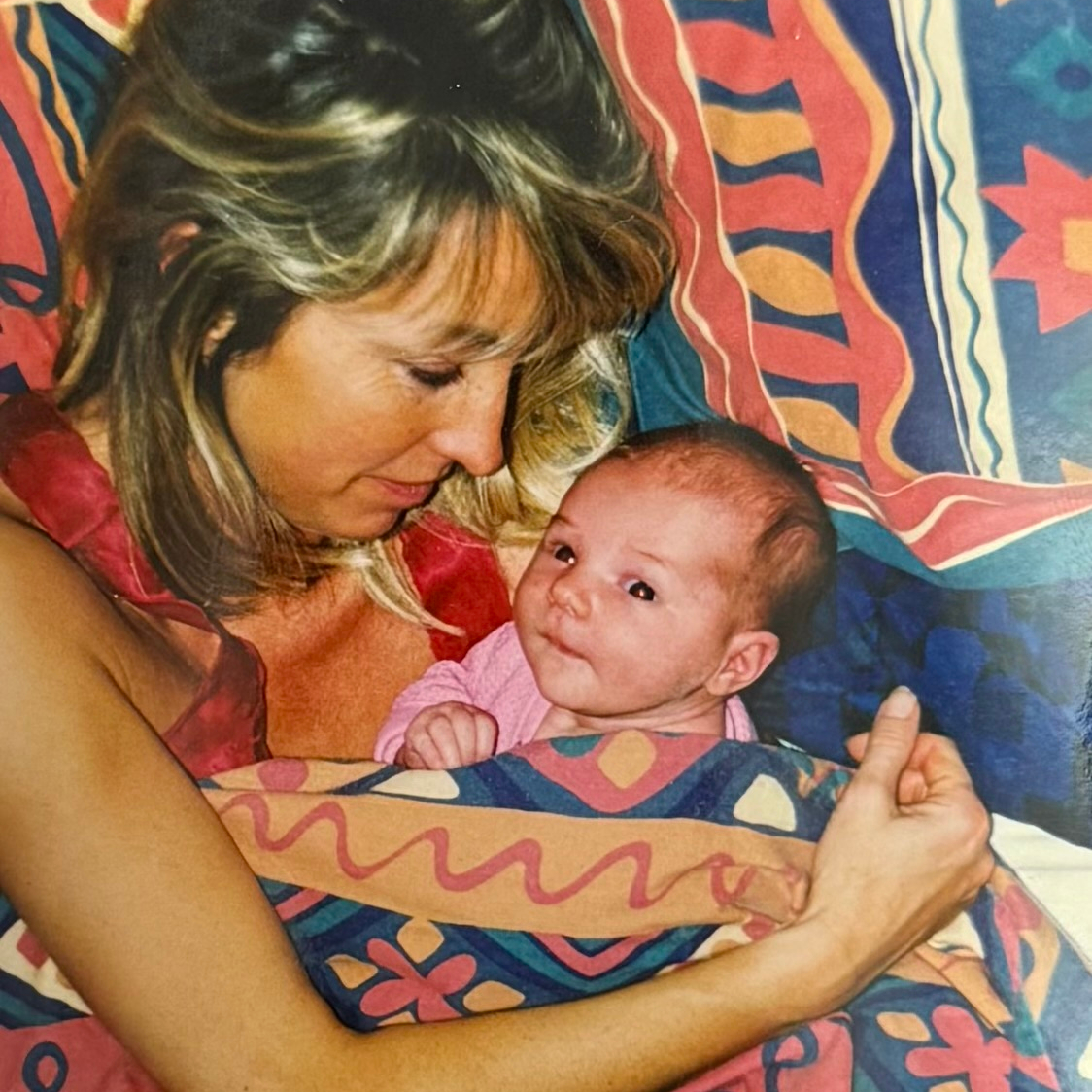
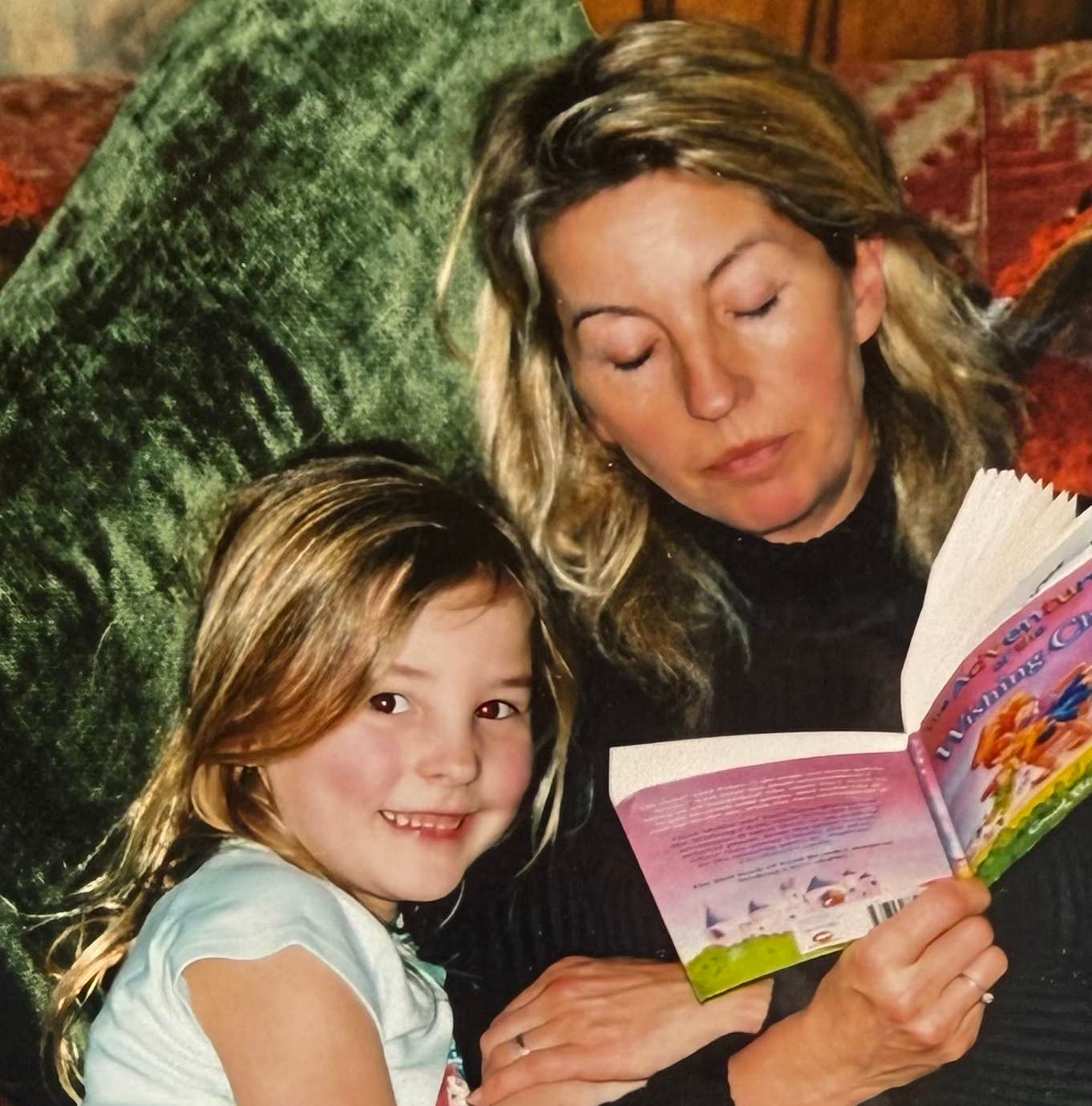
Lily Epps from Hythe was inspired to become a nurse after witnessing the care her mum, Ruth, received from Pilgrims Hospices when Lily was just 18 years old.
Initially training in Brighton, Lily moved home after six months and transferred to Canterbury Christ Church University to support her family after her mum died.
She now works as a Registered General Nurse (RGN) at the Ashford hospice, where her mum died in 2017.
Lily shares why she chose to specialise in palliative care, and what she finds so rewarding about her role.
What drew you to palliative care, and why did you decide to work at Pilgrims Hospices?

My mum was diagnosed with oesophageal cancer when I was 7; she was brilliant and resilient, and outlived an initial three-year prognosis by several years.
After conventional treatment and receiving the all clear, Mum went into remission and began experimental treatments. She worked closely with King’s College Hospital and took part in multiple trials; this fascinated me as I was growing up.
Unfortunately, the treatment didn’t work as we’d hoped, and Mum was referred to palliative care. I remember the Pilgrims nurses coming to visit her in our lounge, they always had an incredible aura of compassion. This really humbled me, and I wanted an opportunity to give back.
My mum always said it was the nurses who would make or break her day, and I strive to be a nurse that makes our patients’ days – especially in their final few days, when it is truly imperative.
I’m lucky and honoured to be part of such an incredible team at Pilgrims; everyone I work with is an inspiration, and so passionate about the care they give.
What does a typical day include for a Pilgrims nurse?
On the in-patient unit (IPU), we start the day with a cuppa to take to handover, which starts at 07:30am. One nurse takes charge and attends morning meetings which includes a whole multidisciplinary team (MDT) meeting, while a second nurse completes the morning medication round.
Depending on patients’ abilities, we’ll help our Healthcare Assistants (HCAs) to shower and bathe them. This is followed by a quick catch-up on the ward so that everyone is aware of any admissions or outstanding jobs, then we tag team going for a quick break before starting the lunchtime medication round.
In the afternoon, we update syringe drivers. We also complete pending discharge paperwork and give any medications needed. We focus on “what matters to me” for each patient, every day; this may be a very small goal, like having a bath, but it can completely change how they feel.
We always try our best to facilitate birthdays and wedding anniversaries. Our catering team provide beautiful cakes that can be enjoyed by families in the garden or in our lovely rooms. Even on long days, the evening quickly comes around, and we enjoy dinner before completing another medication round, settling patients, and handing over to the night staff.
What are the best things about being a nurse at Pilgrims?
Everything is amazing – including the food!
The whole team is incredible, from volunteers to social workers, wellbeing practitioners to consultants. It feels like a family. I’ve never worked anywhere so inclusive; everyone is so lovely, bubbly, down-to-earth and supportive. We all care about the patients and each other, which is clear on a daily basis.
I get more than seven weeks’ holiday per year, which shows how Pilgrims’ care and support extends to staff, too.
They also hold staff celebration days, and twice a year we’re offered therapeutic treatments like massage or reiki that fit around our working day.
What has your role involved and what have you learnt through working at Pilgrims?
I’ve learnt so much in my role at Pilgrims, mostly about different conditions, symptom control and treatment options. Every day is different. Most patients on the IPU come in for symptom control and usually stay with us for around two weeks, whereas the timeframe for our end-of-life patients varies.
I’ve worked with the Outcome Assessment and Complexity Collaborative (OACC) group. This is the collection of data used to measure, demonstrate, and improve the quality of palliative care for patients and their families by assessing clinical outcomes, symptom burden, and the complexity of care.
I also help the team to complete the Integrated Palliative Outcome Scale (IPOS) for patients. An IPOS allows us to integrate our care and ensure we aren’t missing anything, guaranteeing our patients are put first and that we continue to improve and meet their needs.
Do you have any favourite memories or anecdotes from your time at Pilgrims?
Simple things really bring me joy at Pilgrims.

When patients come to us, they’ve often given up; they’ve been bed-bound and stuck inside for weeks. The light in their eyes when you say they can be wheeled outside on their bed and feel the sun on their face again leaves you with no words, and then there’s the cheeky smile when you offer a patient a beer or a glass of wine – these small things make working at Pilgrims so special.
We had an incredible patient who used to be a chef; as part of her legacy, she worked closely with our wonderful occupational therapy team to create a cookbook that is now sold on Amazon and can be shared with her children.
We helped a patient and her daughter do finger prints as part of the patient’s legacy work. The daughter got this as a tattoo in a heart shape, and her mum was able to see it before she died.
We helped to organise a patient’s birthday celebration in their room on the ward. She had two young sons, and one of them had his birthday shortly afterwards, so we did another celebration for him, too.
We decorated their mum’s room whilst she was showering, then surprised her and sang happy birthday; it was a beautiful moment.

One patient, Celia, and her husband, Robert, celebrated their 50th wedding anniversary whilst Celia was in the hospice.
We’d had to remove Celia’s wedding ring because her fingers were swollen. I didn’t want that to be her memory of her final wedding anniversary, so I asked the kitchen to organise a surprise afternoon tea and help me set it up in the garden, and they whizzed up scones and finger sandwiches.
Celia had been bed-bound for a week, but she wanted to go outside, which we discovered via her IPOS (this is why they’re invaluable, and make the hospice so unique). We washed and dressed Celia, then carefully transferred her from her bed into the garden. Robert met us outside with the afternoon tea all set up and decorated just for them.
It’s such a happy place to work; no one wants their final days to be sad, humans are so resilient, and it’s humbling and inspiring being part of the hospice team.

Did you have any preconceptions about hospice care before you worked at Pilgrims?
I was lucky to experience the hospice as a visitor prior to joining the team, as I’d seen first-hand what a joyful environment it is.
People often have the misconception that hospices are all doom and gloom, but in reality they shine such a bright, positive light.
Ukulele singers and Rodney, our prized Pets As Therapy (PAT) dog, fill the ward with smiles and laughter from patients, family and staff.
Of course there are hard days, but they bring the team closer together, as it’s such a supportive environment. There can be hard conversations, too, but you are supported to have them, with the opportunity to debrief afterwards.
Most patients understand why they’re here and just want to enjoy their final days, so it’s important to put them first and try make their wishes come true.
Why is hospice care important?
There is no greater privilege than supporting someone through the final days of their life. Pilgrims promote quality of life; we try our best to ensure patients don’t suffer, supporting them to die with peace and dignity. Although patients are our priority, we’re holistic in our approach; families are an extension of our patients, so when a patient dies, we continue to care for family members who need us.
The services that Pilgrims offer always melt my heart.
Stepping Stones is a bereavement support group run by the wonderful Annie Hogben, Expert Volunteer Development Lead, which is available to any adult living in east Kent, even if their loved one was not a patient of the hospice.
Another element I find so wonderful about Pilgrims is their legacy work; from hand casting and creating family trees, to voice recordings through the Blackbird Project that can be cherished forever.
This is all provided by the charity, which I think is truly incredible, and shows how unbelievably special Pilgrims is.
Pilgrims Hospices is currently recruiting for Registered General Nurses at our Ashford hospice.
If you have relevant experience and have been inspired by Lily’s story, apply today to join our nursing team.